Jul. 31, 2018
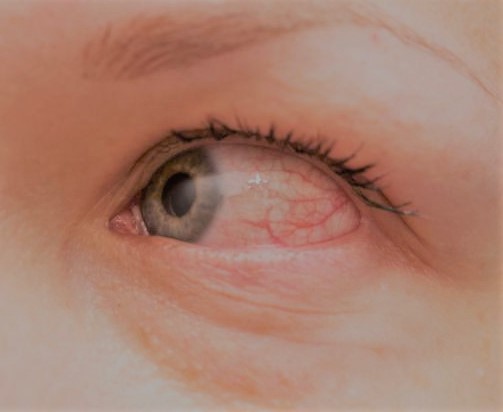
New over-the-counter eye whitening drops may have some advantages over older drops, such as Visine, but ophthalmologists caution that any whitening drops can mask symptoms of serious disease. Lumify was approved by the U.S. Food and Drug Administration in December 2017, and started appearing on store shelves in mid-2018. Ads for Lumify state the drops can be used four times a day. However, anyone who thinks they need drops that often should first have their eyes checked by an ophthalmologist to find out what's causing the redness, says Laurie Barber, MD, a spokesperson for the American Academy of Ophthalmology.
The active ingredient in Lumify is brimonidine, which was first approved by the FDA in a higher dose as a prescription glaucoma drug called Alphagan. Visine's active ingredient is tetrahydrozoline. Both drugs work to reduce eye redness by causing constriction of the blood vessels in the eye, decreasing both blood flow and oxygen getting to the eye's tissue.
Once a person stops using drops containing tetrahydrozoline, the blood vessels are no longer constricted. As vessels open again, they can become even larger than before, as nutrients and oxygen return to the eye. The enlarged arteries pump more blood to make up for lost time, which can cause increased redness in the eyes—called the rebound effect. This can lead to a cycle where people depend on the drops to have clear, white eyes.
The key difference in the way the two drugs work is that Visine targets a receptor in the eye's arteries, while Lumify acts on a receptor in the veins. The arteries carry oxygen-rich blood to the eye, while the veins take blood away from the eye. By targeting the veins, Lumify doesn't interrupt oxygen flow to the eye, reducing the risk of a rebound effect, according to Bausch & Lomb, who makes the drops.
Dr. Barber says she has questions about Lumify’s long-term effects, since the studies used by the FDA to approve the drops lasted only five weeks. She also notes that the drops contain a preservative called benzalkonium chloride, which can cause a reaction in the eye. "If you’re using Lumify four times a day, you’re putting a lot of preservative in your eye," she says.
Dr. Barber's biggest concern with any eye-whitening drops is that a person may use them to get rid of redness that may be a symptom of eye disease. Eye redness can be associated with a wide range of conditions, including allergies, conjunctivitis (pink eye), corneal ulcer, glaucoma and bleeding in the eye.
"I would prefer that patients not use an eye-whitening drop on a regular, long-term basis. But, for short-term use on an occasional basis, Lumify is purported to have less rebound redness," she said. "We don’t want patients to use eye drops that mask symptoms of their disease—if there is something wrong with the eye, we need to know about it. A person should get evaluated for red eyes before using eye drops on a regular basis."